Myotherapy can help you rapidly overcome the pain and disability of disc bulge to achieve a pain free life – using manual therapy, education and the correct movement strategy. Disc bulge is not a life sentence – our Myotherapists will treat your pain so you can move easily and recover quickly.
We care about disc bulge and people in pain. This article describes the best ways to efficiently reduce pain associated with disc bulge using a combination of scientifically validated techniques – including hands on therapy and using the correct movement strategy.
In too much pain to read the article (2 min reading time) – hit the book now button to rapidly reduce your pain.
Most disc bulges are very straight forward to treat. Why do so many people report severe pain and loss of quality years after disc bulge?
- Extended bed rest and the use of opioids for pain relief prolongs the damage caused by bulging disc.
- When symptoms start is when inflammatory chemicals are the MOST destructive. You need to move to remove these chemicals with blood flow.
- Effective movement strategies, targeted manual therapy and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
- Knead Myotherapy provide an effective non-surgical opioid free strategy to overcoming bulging disc pain and sciatica. Our expert Myotherapists won’t just treat your symptoms – they’ll show you how to quickly overcome the CAUSES of bulging disc pain, radiculopathy and sciatica.
What causes bulging disc?
The majority of bulging discs are caused by accumulated low load trauma – repeated small load maintained for a long time. Research has shown that individuals that are desk bound for much of the day are at a higher risk of disc bulge than those in active jobs.
One analogy about how the “shell” of the disc starts to weaken is a little like metal fatigue. If you fold a piece of tin repeatedly, eventually the fold separates. What this means for the disc is that the moment you “bulge the disc”, is only the conclusion of an ongoing process.
People statistically more likely to experience bulging disc:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
- Have a previous history of back pain
- Are aged between 40-69 (the 50’s is the highest risk age group of female gender)
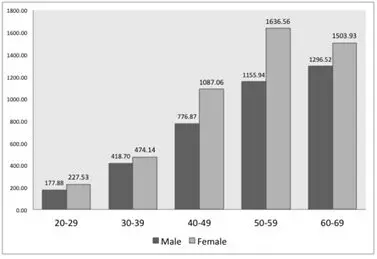
Incidence of disc bulge by age and gender taken from Differences in the Incidence of Symptomatic Cervical and Lumbar Disc Herniation According to Age, Sex and National Health Insurance Eligibility: A Pilot Study on the Disease’s Association with Work
By Kim et al (2018) retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6210730/figure/ijerph-15-02094-f001/
What does bulging disc feel like?
A common Google query is – what bulging disc symptoms?
Typically Symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
What should you do for disc bulge Brisbane?
One of the most common questions we’re asked about disc bulge is – how to cure disc bulge?
The direction that the disc displaces will affect the symptoms and pain significantly. The first thing is to determine which postures an individual can tolerate without pain and base the movement strategy off those.
- KEEP MOVING – Extended bed rest and the use of opioids for pain relief have been shown to extend the duration of bulging disc pain significantly – MONTHS BECOME YEARS.
- During the acute phase (immediately after symptoms start) is when pain and inflammatory chemicals are the most Find an exercise you like doing that doesn’t hurt – swimming, walking, cycling, lawn mowing and do it.
Targeted hands on manual therapy can provide immediate relief to muscle spasm caused by disc bulge – assisting you to move without pain.
World leading authority Prof Stuart McGill cites fast walking as generally therapeutic regardless of the direction of disc bulge.
The reasons are:
- reduction of pain generating inflammatory chemicals
- tissue load sharing
- more upright posture
- gentle motion
- reduced spine loads and greater core activation from fast arm swing.
These benefits do not occur during slow walking or mall strolling, which often makes symptoms worse because of insufficient core activation and increased spinal pressure.
What shouldn’t you do?
Don’t endlessly try to stretch your back and hamstrings – most disc bulges have nerve injury, you can’t stretch away nerve pain – the relief is temporary and is attributed to the stretch reflex releasing some feel good neurotransmitters. It’s actually irritating the nerve more.
Try not to assume only one sitting posture – numerous studies have shown that variable sitting postures are better because they don’t overload any one tissue structure.
Try to do things you enjoy – Stress elevates inflammatory chemicals. Try to enjoy life by finding activities that give pleasure. Disc bulge is not a life sentence – even in sedentary people, statistically they shrink within 2 years.
Maintain good sleep hygiene – when normal sleep returns, emotional resilience grows and inflammation reduces.
How herniated disc is treated?
How does bulging disc heal? Pain is different for every individual – what helps one person will inflame another. Determining the direction of the bulge is the most important factor – as this will show you which positions you can build strength and endurance in.
Every tissue within the body requires movement for healthy function. No load and too much load are equally bad – finding the right amount of load for your present capacity is the way to accelerate recovery.
A typical initial disc bulge treatment will involve:
- assessment of movement quality
- finding what positions increase pain
- finding out which movements reduce pain
- manual therapy to reduce muscle guarding
- nerve glides to reduce neural inflammation and improve blood flow
- Lo Level Laser – to reduce harmful inflammation and promote the healing benefits of beneficial inflammation
- electro needling (if necessary) to calm angry inflamed pain generating nerves – stopping shooting pain down the arm or legs)
- a program of movements designed to improve muscular endurance (and for low back pain) gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles).
What is meant by disc bulge?
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebr
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
Related Posts

SIJ Pain Brisbane

Sciatica Pain Treatments
Frequently Asked Questions (FAQs)
The two names are used to indicate severity. A bulging disc may not have much material escaping the disc, wheras a herniated disc will have a large amount of spill. A third term prolapsed disc also exists indicating significant loss of disc fluid.
Between the ages of 40-60 sties have shown approximately 8% of the population have symptomatic disc bulge.Between the ages of 20-40 less than 3% of the population have been shown to have symptomatic disc bulge.
Less than 1% of the population are estimated to suffer from symptomatic bulging discs in the neck (cervical spine). Peak incidence occurs between the ages of 40-60.
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
The majority of disc bulges are conditions that will become non symptomatic within 6-24 months – if you keep moving. Serious disc bulges include conditions where bladder and bowel control are affected and paralysis of the legs are present. If you experience low back/neck pain or shooting pain in the extremities – it is important to consult a health professional that deals with these conditions.
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Absolutely yes. If a bulge is large enough it can press on multiple regions of the spine and cause referred pain, weakness, numbness down both legs.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Absolutely yes. Nerve compression from L1-3 often radiates into the groin. Your Myotherapist should be able to provide treatments and exercises to rapidly reduce discogenic pelvic pain.
Disc bulge is a common cause of sciatica. The bulging material comporesses nerves as they exit the spine (or the spine itself) and this causes sensations, such as numbness, tingling, pain and even weakness or paralysis down the leg.
It is easy to irritate symptomatic disc bulge by performing movements that irritate the tissues. Finding out which movements are therapeutic and which inflammatory is one of the best ways to speed recovery. Consult with your Myotherapist early.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Dizziness is not a standard symptom of disc bulge. Theoretically a disc bulge in the neck can be so painful that the pain signals are perceived by other nerves in the head such as the vestibulocochlear nerve (the balance/hearing nerve). This cross talk is unlikely and if you are experiencing dizziness suddenly you should immediately seek out a GP.
Absolutely. Any irritation of the vertebrae of the neck can cause cervicogenic headache – a type of headache caused by irritable nerves in the neck. Another possible headache trigger caused by a bulging disc in the neck could be a simple tension headache. Seek out your Myotherapist for rapid resolution of cervicogenic and tension headaches.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
Yes. Any paralysis should be treated as a life threatening emergency – call 000 immediately.
Disc bulge is a common cause of sciatica. The bulging material comporesses nerves as they exit the spine (or the spine itself) and this causes sensations, such as numbness, tingling, pain and even weakness or paralysis down the leg.
It is easy to irritate symptomatic disc bulge by performing movements that irritate the tissues. Finding out which movements are therapeutic and which inflammatory is one of the best ways to speed recovery. Consult with your Myotherapist early.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Dizziness is not a standard symptom of disc bulge. Theoretically a disc bulge in the neck can be so painful that the pain signals are perceived by other nerves in the head such as the vestibulocochlear nerve (the balance/hearing nerve). This cross talk is unlikely and if you are experiencing dizziness suddenly you should immediately seek out a GP.
Absolutely. Any irritation of the vertebrae of the neck can cause cervicogenic headache – a type of headache caused by irritable nerves in the neck. Another possible headache trigger caused by a bulging disc in the neck could be a simple tension headache. Seek out your Myotherapist for rapid resolution of cervicogenic and tension headaches.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
Yes. Any paralysis should be treated as a life threatening emergency – call 000 immediately.
Disc bulge is a common cause of sciatica. The bulging material comporesses nerves as they exit the spine (or the spine itself) and this causes sensations, such as numbness, tingling, pain and even weakness or paralysis down the leg.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Usually – yes.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
It is possible – but it takes a long time. Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Whaterver makes you happy and doesn’t increase pain. World leading authority Prof Stuart McGIll cites fast walking as generally therapeutic regardless of the direction of disc bulge.
The reasons are:
- reduction of pain generating inflammatory chemicals
- tissue load sharing
- more upright posture
- gentle motion
- reduced spine loads and greater core activation from fast arm swing.
These benefits do not occur during slow walking or mall strolling, which often makes symptoms worse because of insufficient core activation and increased spinal pressure.
Whaterver makes you happy and doesn’t increase pain. World leading authority Prof Stuart McGIll cites fast walking as generally therapeutic regardless of the direction of disc bulge.
The reasons are:
- reduction of pain generating inflammatory chemicals
- tissue load sharing
- more upright posture
- gentle motion
- reduced spine loads and greater core activation from fast arm swing.
These benefits do not occur during slow walking or mall strolling, which often makes symptoms worse because of insufficient core activation and increased spinal pressure.
Studies have shown that over a period of months disc material is broken down and reabsorbed by the body. This means that over time disc bulges shrink. Pain becomes chronic – when people do not find the best movement strategy to optimise this re-absorption process and allow their muscles to atrophy. Early movement strategies reduce destructive inflammation that lead to chronic pain caused by damage to slow healing tissue such as ligaments, joints and nerves.
Studies have shown that over a period of months disc material is broken down and reabsorbed by the body. This means that over time disc bulges shrink. Pain becomes chronic – when people do not find the best movement strategy to optimise this re-absorption process and allow their muscles to atrophy. Early movement strategies reduce destructive inflammation that lead to chronic pain caused by damage to slow healing tissue such as ligaments, joints and nerves.
Studies have shown that over a period of months disc material is broken down and reabsorbed by the body. This means that over time disc bulges shrink. Pain becomes chronic – when people do not find the best movement strategy to optimise this re-absorption process and allow their muscles to atrophy. Early movement strategies reduce destructive inflammation that lead to chronic pain caused by damage to slow healing tissue such as ligaments, joints and nerves.
- finding what positions increase pain
- finding out which movements reduce pain
- manual therapy to reduce muscle guarding
- nerve glides to reduce neural inflammation and improve blood flow
- electro needling (if necessary) to calm angry inflamed pain generating nerves – stopping shooting pain down the arm or legs)
- a program of movements designed to improve muscular endurance and for low back pain gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
Usually – yes by:
- finding what positions increase pain
- finding out which movements reduce pain
- receiving manual therapy to reduce muscle guarding
- using nerve glides to reduce neural inflammation and improve blood flow
- applying electro needling (if necessary) to calm angry inflamed pain generating nerves – stopping shooting pain down the arm or legs)
- following a program of movements designed to improve muscular endurance and for low back pain gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles
A vertebral disc is a spongy fluid filled capsule that sits between each vertebra The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads. A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through. The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs. This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- finding what positions increase pain
- finding out which movements reduce pain
- manual therapy to reduce muscle guarding
- nerve glides to reduce neural inflammation and improve blood flow
- electro needling (if necessary) to calm angry inflamed pain generating nerves – stopping shooting pain down the arm or legs)
- a program of movements designed to improve muscular endurance and for low back pain gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles
- finding what positions increase pain
- finding out which movements reduce pain
- manual therapy to reduce muscle guarding
- nerve glides to reduce neural inflammation and improve blood flow
- electro needling (if necessary) to calm angry inflamed pain generating nerves – stopping shooting pain down the arm or legs)
- a program of movements designed to improve muscular endurance and for low back pain gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles
- finding what positions increase pain
- finding out which movements reduce pain
- manual therapy to reduce muscle guarding
- nerve glides to reduce neural inflammation and improve blood flow
- electro needling (if necessary) to calm angry inflamed pain generating nerves – stopping shooting pain down the arm or legs)
- a program of movements designed to improve muscular endurance and for low back pain gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles
-
This term is not accurate. Discs burst, they do not move.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
- A vertebral disc is a spongy fluid filled capsule that sits between each vertebra
- The capsule can lose its flexibility as a part of aging or by exposure to sustained postures over a long period (desk workers have a higher rate of disc bulge than manual workers), or from frequently lifting heavy loads.
- A type of tissue fatigue occurs in the capsule wall which creates a weakness that may allow the liquid contents to burst through.
- The paste inside then frequently presses against the spine or spinal nerve roots causing pain the refers down the arms or legs.
- This paste will start a process of inflammation that is destructive to other types of tissues, such as ligaments and nerves. Causing the long standing pain associated with disc bulge.
You should NOT consider surgery unless you have had serious debilitating pain that does not respond to movement for more than 12 months. The literature is clear – early surgery is not a good option for the majority of bulging discs and usually leads to chronic pain states.
If you experience paralysis or are unable to walk.
This is highly variable. Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
Bulging discs can occur anywhere in the spine. They most commonly occur in the low back L4/5 L5/S1 – causing low back pain and shooting pains down the legs. They also occur less commonly in the neck wher they can cause pain to radiate down the leg and a condition called discogenic wry neck – an inability to move the neck a certain way.
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
- Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
A Myotherapist is a perfect clinician to resolve bulging disc rapidly. Your Myotherapist will:
- find what positions increase pain
- find out which movements reduce pain
- provide manual therapy to reduce muscle guarding
- show you nerve glides to reduce neural inflammation and improve blood flow
- use proven techniques such as electro needling to reduce shooting pain down the arms or legs
- develop a program of movements designed to improve muscular endurance and (for low back pain) gluteal function (low back pain inhibits gluteal function increasing load on the injured low back muscles).
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
This is highly variable. IT is common for people to have disc bulges on MRI and report NO symptoms. However symptomatic disc bulge can cause significant pain and dysfunction.
Typically symptoms of disc bulge include:
- Weakness in the arms or legs from spinal nerve compression or irritation.
- Radiating pain – shooting arm pain or shooting pain down leg (radiculopathy)
- Severe back pain and or shooting pain down leg (sciatica) – shooting pain is frequently felt in the calf also.
- Neck pain or tingling/numbness in neck
- Inability to move the neck (wry neck)
Muscle Spasm – in the neck, arms or back and legs (caused by inflammatory chemicals saturating the nerves)
Why herniated disc treatment?
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens.
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens.
Discs burst they don’t move.
The majority of bulging discs are caused by accumulated low load trauma – repetitive load maintained for a long time. An analogy is a little like metal fatigue – fold a piece of tin repeatedly and eventually the fold weakens. People statistically at risk of disc bulge:
- Are sedentary – spending more than 6 hours per day sitting
- Carry extra weight
- Spend 2 hours a day or more in a vehicle (vibration while seated increases the likelihood bulging a disc)
Are aged between 40-69
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
That depends on the severity of the injury and whether or not the individual maintains activity and uses opioids. Extended bed rest and the use of opioids have been shown to extend the duration of bulging disc pain significantly.
Multiple studies have shown that the majority of disc bulges have shrunk within 2 years. This time can be drastically reduced with appropriate movement strategies and early intervention.
Ongoing pain after this time is usually linked to destructive inflammatory chemicals compromising tissues in the early acute stages causing – ligament damage, arthritic change (osteoarthritis in the joints), nerve dysfunction and central sensitisation (neuroplastic change where the body becomes efficient at making pain). Effective movement strategies and low level laser are proven to reduce destructive inflammatory chemical that damage slow healing soft tissue such as nerves and ligaments.
An already irritable disc bulge is unlikely to reoccur after 3 years when the bulge has been reabsorbed.
However pain in the low back may become chronic after disc bulges – especially if inflammatory chemicals damage tissues such as ligaments, nerves and vertebral joints. Ongoing pain after 3 years is usually caused by an incorrect management strategy when the disc injury happened – such as extended bed rest and the use of opioids.
X-rays and CT scans are not sensitive to cartilage type tissues such as discs. If you need to get imaging for a disc bulge you need an MRI.
https://uwaterloo.ca/kinesiology/hes-got-our-backs
https://www.bbc.com/future/article/20160418-the-surprising-downsides-of-sit-ups
https://www.livestrong.com/article/392341-stuart-mcgills-big-three-back-exercises/
https://www.abc.net.au/science/articles/2000/01/17/93512.htm
https://www.abc.net.au/news/2010-05-01/pain-in-the-neck–woods-will-have-tests-to/428270?nw=0
https://abcnews.go.com/Health/CommonPainProblems/story?id=4047844
https://www.ncbi.nlm.nih.gov/books/NBK441822/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5685963/
https://www.health.harvard.edu/a_to_z/herniated-disk-a-to-z
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7010513/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6147874/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5521897/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3743527/

Roger Morelli








Latest posts by Roger Morelli (see all)
- Wrist RSI - July 3rd, 2024
- Carpal Tunnel Treatment Brisbane - July 3rd, 2024
- Deep Tissue Massage Brisbane - July 3rd, 2024